African healthcare is shifting from one-size-fits-all delivery to fine-tuned, data-driven care that reflects real lives, real environments and fundamental biology. Personalised health in Africa is undergoing a quiet revolution, and the future looks promising.
It is no longer just about building more clinics or speeding up drug deliveries. Artificial intelligence (AI) is enabling personalisation—routines, diets, skincare, and wellness plans that are not generic, but tailored to African skin, diets, climates, and daily realities. For a broader tour of tools and trends, see our guide to AI in health & wellness across Africa.
In this article, we demonstrate how AI personalises wellness, identify the major players, explain why skincare serves as a pragmatic gateway to broader health optimisation, and outline what lies ahead if startups and public systems align.
What “personalised health in Africa” means
Personalised health adapts care to the individual; in Africa, the differences are amplified by biology, climate and culture.
“Personalised health” is care that takes into account genetics, environment, lifestyle, skin type, diet, and climate. In Africa, these variables do more than nudge outcomes—they reshape them:
Skin diversity and UV exposure. Many dermatology datasets have historically been biased toward lighter skin tones, which has weakened diagnostic performance for pigmented skin. The PASSION for Dermatology project, for example, assembled 4,901 images from 1,653 patients across sub-Saharan Africa to correct that bias and improve models on common paediatric conditions (eczema, fungal infections, scabies, impetigo). This is what it looks like to build AI that actually “sees” African skin.
Dietary diversity—characterised by staple patterns such as maize, sorghum, millet, cassava, yams, and pulse-rich cuisine—shapes gut microbiomes and micronutrient gaps differently from Western dietary patterns. Personalised nutrition built on Western food logs and portion sizes often misfires without local calibration.
Environmental realities, including heat, humidity, dust, air pollution, water quality, and endemic pathogens, affect skin barrier function, respiratory stress, hydration, and disease risk. Context-aware models that ingest UV, temperature/humidity and pollution data make more appropriate recommendations.
The point is simple: personalisation is not a luxury add-on; it is the difference between advice that works and advice that reads well but misses the mark.
How AI is personalising wellness: skin, diet and environment
The mechanism: AI turns fragmented signals into patterns, then translates those patterns into actions that follow the best course for real people.
Skin & skincare
Opening move: Dermatology is where African personalisation has made the clearest early gains.
- Bias-aware computer vision (CV): Teledermatology models trained with African images (e.g., PASSION) markedly improve detection and referral quality for darker skin tones. This does not replace clinicians; it prioritises who needs a faster review and what evidence to capture.
- Data-led skincare brands: Uncover (Kenya) combines selfie analysis, micro-surveys, and environmental signals (UV, humidity, pollution) to recommend personalised routines for melanin-rich skin (learn how to personalise your skincare with AI). The logic is not a mystery: when the model has seen a Lagos rainy season and a Nairobi dry spell, it recommends differently.
- Feedback loops: Users record breakouts, irritation, or improvements; the system learns which actives (e.g., niacinamide vs. azelaic acid) and which textures (gel vs. cream) perform better under specific climatic conditions and skin types.
Diet, nutrition & lifestyle
Second layer: Food and routine adjustments compound small gains into sustained outcomes.
- Dietitian copilots: AI assistants help practitioners translate local staples into adequate protein, fibre and micronutrient coverage—without prescribing unrealistic imports.
- Population-level analytics: Predictive models flag nutrition stress and outbreak risk for planners and community health workers, targeting limited resources to where they can have the most significant impact.
New to meal planning? We tested the best AI meal planners for beginners.
Environment-aware nudges
The daily edge: Micro-context, delivered just in time, changes behaviour.
- UV- and humidity-aware coaching: On high-UV days, the app may encourage users to use zinc oxide sunscreen and increase hydration; on dusty, harmattan afternoons, it may recommend barrier-supporting routines.
- On-device inference: For low-bandwidth areas, lightweight models run offline and sync later—crucial for reliability when power or data is patchy.
For the policy rails behind this shift, our African AI adoption roadmap breaks down standards, data rights and interoperability.
Local startups leading the revolution (narrative, not a table)
Ecosystem view: These teams don’t all solve the same problem; together, they form the stack of personalisation needs.
Reliance Health (Nigeria)
Why it matters: Reliance built the “rails” on which personalisation can run at a population scale.
Reliance Health integrates telemedicine, insurance, diagnostics and pharmacy under one roof. This architecture enables AI to perform practical tasks, such as NLP symptom intake for triage, risk scoring for chronic conditions, and routing to the appropriate clinician, lab, or medication.
The company raised $40 million in Series B funding to expand its full-stack model. Personalisation works best when the entire patient journey—which consists of consultations, tests, medications, and follow-ups—can be tailored, not just a single step.
Uncover (Kenya → Pan-Africa)
Why it matters: Uncover proves that skincare is a credible gateway into broader health.
Uncover is a data-driven brand for melanin-rich skin that utilises selfies, micro-surveys, and climate data to personalise routines, while blending African botanicals with Korean R&D.
The brand’s growth narrative explicitly emphasises technology and data. More importantly, it demonstrates a scalable path: start with a high-engagement entry point (skin), earn trust, collect consistent outcomes data, and then expand toward hormonal and lifestyle guidance.
Vezeeta AI (Egypt & Pan-Africa)
Why it matters: Vezeeta shows the operational side of AI—matching, logistics, prescriptions.
Vezeeta evolved from appointment booking into data-driven care matching and e-pharmacy logistics. Its AI features support doctor-patient matching, no-show prediction and prescription optimisation.
An innovation hub (“Vezeeta Lab”) formalises that pipeline—a reminder that personalisation also means the proper care, at the right time, with the right medicine.
AHADI (Pan-Africa)
Why it matters: Without African data, personalisation is an imported guess.
The African Health Analytics & Data Initiative focuses on collecting, cleaning, and sharing local health data, enabling startups and researchers to train models that effectively perform in African populations.
It is less glamorous than a new app, but it is the load-bearing beam: without local data, imported models misdiagnose, overfit or exclude.
Skincare as a gateway to broader health optimisation
The bridge: Skin is visible, frequent and culturally salient—making it an ideal onboarding path for health tech.
In many African contexts, acne, hyperpigmentation, eczema and fungal conditions shape self-confidence, social life and employment prospects. Because outcomes are visible, people engage early and often.
That engagement generates high-frequency, high-quality data: what was used, in what climate, on what skin, with what result. From there, it is a short step to nutrition prompts (such as increasing zinc or omega-3 intake), hydration targets on hot days, hormone-aware scheduling, and preventive testing nudges tied to family history.
In other words, skincare is not superficial; it’s the door handle to a home full of health improvements.
The AI under the hood (plain English)
Transparency matters: Users and clinicians should understand what these systems actually do.
- NLP triage & routing: Symptom text is fed into models that classify urgency and suggest next steps, then matched to a GP, specialist, lab, or pharmacy.
- Risk scoring: Tabular models estimate flare risk (e.g., for hypertension/diabetes), no-show probability, and adherence likelihood given travel distance, pay cycle and prior behaviour.
- Computer vision for skin: Convolutional/transformer models detect acne, hyperpigmentation and texture issues on darker skin tones, trained with pigment-aware datasets (e.g., PASSION).
- Recommenders: A rules-plus-ML blend considers skin type, diet, climate, and prior outcomes to recommend the best course of action—from sunscreen texture to when to schedule a lab test.
- Low-connectivity engineering: On-device inference, offline capture with later sync, and SMS/USSD/IVR fallbacks. This is not optional; it is what responsible African deployments look like.
The complex parts—no sugar-coating
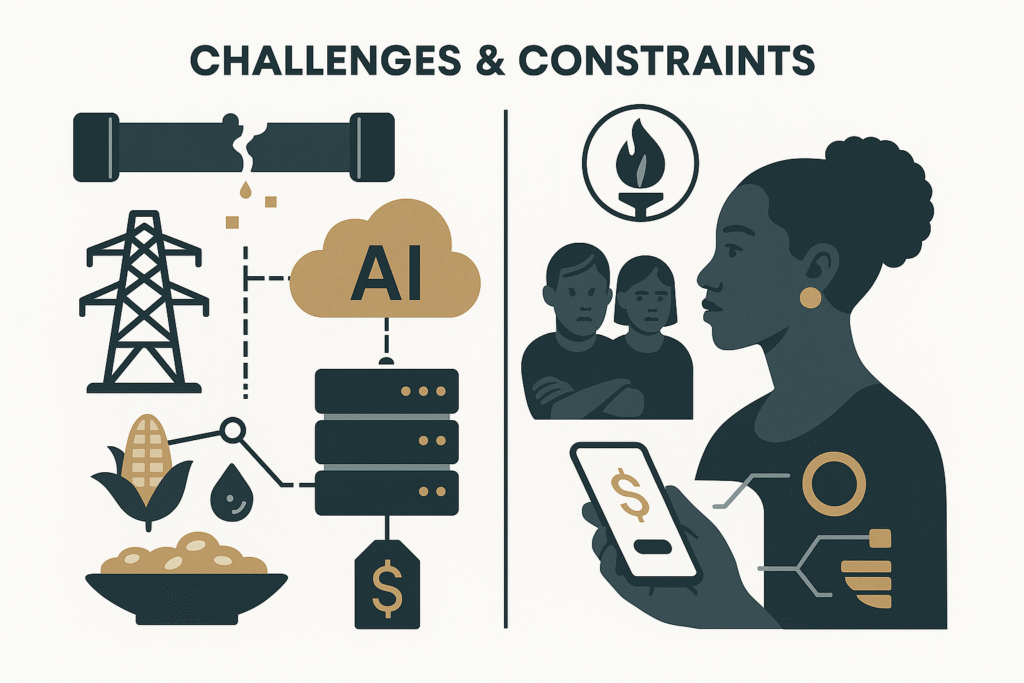
Reality check: Personalisation only scales if we confront five constraints head-on.
- Data gaps & bias: Most historical datasets are Western. Dermatology is improving (PASSION), but nutrition, genomics and microbiome data remain thin. The fix is slow and deliberate: collect local ground truth and evaluate fairness on local sub-populations.
- Infrastructure reality: A significant share of health facilities report unreliable electricity, and connectivity can be fragile outside major cities. Design must account for power cuts and low bandwidth; otherwise, systems will operate effectively in pilots but fail at scale.
- Regulation & trust: People deserve explicit consent and control over their data. WHO guidance stresses transparency, risk management and post-deployment monitoring for health AI. Building trust is not a marketing task; it is an architecture and process task.
- Affordability & access: Smartphone affordability and data costs remain barriers for many households. That is why responsible teams ship good USSD and IVR experiences and consider community health worker workflows, not just glossy apps.
- Cultural fit: Advice that ignores language, food culture or gender norms will underperform. Personalisation only works if it honours local realities, from pay cycles to staple foods to climate rhythms.
How public health systems can integrate AI—without breaking
Institutional path: Ministries and hospital networks can integrate AI personalisation into the system, rather than treating it as a side project.
A) Lay the rails first (records + standards)
Why this is first: Without the pipes, nothing flows.
Digitise records (EHRs) and enforce interoperability (e.g., FHIR-style endpoints) so startups can plug in safely. Build a national, de-identified health data layer with role-based access, audit trails and breach protocols. This is how you turn fragmented visits into coherent longitudinal care.
B) Start with high-volume, low-risk use cases
Why this sequence: Win where the numbers are big and the risk is controlled.
Begin with nurse-line triage, no-show prediction, and chronic-disease risk flags for community health workers. Pilot, evaluate, publish the results, then scale. Rwanda’s long-horizon partnership model serves as a valuable reference point, featuring a staged rollout, shared metrics, and public oversight.
C) Design for low-resource realities
Why this matters: The grid won’t adapt to your app.
Mandate SMS/USSD/IVR access, edge-friendly models and offline sync. If an AI tool dies every time there is a power cut, it is not a health product; it is a prototype.
D) Keep clinicians and patients in the loop
Why this protects outcomes: AI is a copilot, not an autopilot.
Set up Model Review Boards in teaching hospitals. Require explainable artefacts (i.e., why this suggestion, which features mattered) and simple override controls. Train staff to confidently accept or reject suggestions, and embed post-market surveillance to detect drift and bias.
E) Procure outcomes, not hype
Why this aligns incentives: Pay for health, not for slide decks.
Contracts should specify measurable endpoints, including reduced time-to-diagnosis for dermatology referrals, adherence lift in hypertension clinics, decline in emergency admissions per 1,000 population, and equity metrics (such as urban vs. rural, language groups, and gender).
Future developments of personalised health in Africa
Looking ahead: Three frontiers will push personalisation deeper and broader.
1) Genomics & microbiome personalisation
Why it matters: African populations hold the world’s most extraordinary genetic diversity—currently under-represented in global datasets.
Expanding Africa-led genomics will unlock drug-response predictions and disease-risk stratification that reflect local genetics. In parallel, research on skin and gut microbiomes will move beyond cosmetics into areas such as immune regulation, metabolic health, and infection resilience. Expect startups to partner with universities and public labs to make precision health locally valid and affordable.
2) Predictive & preventive public health
Why does it change the curve? Early signals beat heroic rescues.
By fusing weather, mobility, wearable and clinic data, ministries can build early-warning dashboards for outbreaks and nutrition stress—acting weeks earlier than today. On the individual level, risk models will encourage families to adopt low-cost preventive measures (BP checks, glucose monitoring, heat-health routines) before a crisis occurs.
3) AI health coaches in local languages
Why this scales access: The cheapest clinic is the one on your phone.
Imagine AI companions in Hausa, Swahili, Yoruba, Amharic, or Pidgin that adjust hydration targets on high-UV days, recommend alternative staple swaps to improve micronutrient coverage without increasing costs, and send time-based medication reminders to align with pay cycles and commute patterns.
The best of these will work on entry-level Android, USSD or IVR—because equity is a distribution problem as much as a modelling problem.
Long-term impact if we get it right
The pay-off: Personalisation shifts care left—earlier, cheaper, fairer.
- Earlier detection and fewer severe episodes: AI triage and risk flags expedite diagnosis; pigment-aware CV reduces missed dermatology referrals for darker skin.
- Higher adherence and continuity: Reminders tuned to language, transport and pay cycles reduce no-shows and medication drop-off—the quiet killers of chronic-disease programmes.
- Better resource targeting: Staff and diagnostics concentrate on high-risk cohorts; predictive pharmacy logistics reduce stock-outs and wasted spend.
- Equity by design: Local datasets and multilingual UX narrow gaps between urban and rural areas, men and women, and majority and minority language groups—provided bias checks and affordability are enforced.
- Public health intelligence: Aggregated, de-identified signals from symptom chats, skin images, and vital signs feed real-time dashboards, improving outbreak and heat health responses.
Mental health is part of the same arc; here’s how 24/7 AI support works.
Personalisation is not a gadget; it is a systems upgrade. When it works, it bends the care curve toward earlier, cheaper, and fairer care.
Practical checklist—for founders and officials
Make it actionable: Here’s a compact playbook you can actually execute.
For startups
- Build for offline/low-power use first; do not add it later.
- Collect local ground truth (skin images, diet baselines, vernacular text) with consent that people can understand.
- Ship model cards: intended use, limits, fairness checks, retraining cadence.
- Prove outcomes in weeks, not years: adherence lift, time-to-diagnosis cuts, pharmacy stock-out reduction.
For ministries and hospital networks
- Invest in EHRs + interoperability; make API access a procurement requirement.
- Establish Model Review Boards and mandate explainability and override mechanisms.
- Procure against clinical endpoints and equity metrics; publish results.
- Align with ethics guidance and continental data-governance efforts; fund local analytics capacity (e.g., AHADI and university labs).
Key takeaways
The short version: What to remember when the tabs are closed.
- Local first, then scale: African data, languages, diets and climates in the loop—otherwise personalisation is theatre.
- The ecosystem is forming: Reliance Health (platform rails), Uncover (skincare gateway), Vezeeta (matching and e-pharmacy), AHADI (data backbone).
- Governments unlock durability by funding records, standards, and connectivity; piloting high-volume use cases; and procuring based on outcomes.
- Next frontier: Genomics, prevention and multilingual AI companions push personalisation from beauty and diet into mainstream primary care.
Conclusion
AI has the potential to transform wellness in Africa from a one-size-fits-all model into something deeply personal, culturally meaningful, and more effective.
Skincare is one of the early success stories—because skin is visible, people care, and small wins matter. But the real prize is when this personalisation ripples out: better nutrition, earlier detection of illness, smarter public health, and for each person, wellness that fits their life, not someone else’s template.
The future isn’t inevitable. It depends on who builds the tools, how data is collected, how ethical frameworks are established, and whether the economic models include—not exclude—the many pathways people use to take care of themselves. If those align, AI in Africa can power a wellness revolution.